The cobas® HPV Test is the only clinically validated, FDA approved, genotype-based test for HPV primary screening. The test simultaneously detects 14 high-risk HPV types and provides specific genotyping information for HPV types 16 & 18. Then a pooled result on the twelve other hrHPV genotypes. This allows genotyping to take place during co-testing. NO OTHER HPV TEST DOES THIS! Eliminates one stage of reflex testing.
• Internal control insures adequacy of the sample
• Decreases false negative and false positive rates compared to Pap alone
• Results are unequivocal and objective
• Test detects cause of cervical cancer rather than nonspecific cellular changes
This is combined with the STD Panel: Chlamydia, Gonorrhea, Trichomonas, HSV, Bacterial Vaginosis (BV), Candida Vaginitis (CV) and HPV.
The Society of Gynecologic Oncology (SGO), the American Society for Colposcopy and Cervical Pathology (ASCCP), with input from representatives of five other US national medical organizations (ACOG, ACS, ASCP, ASC, CAP) issued an Interim Guidance Report1 in early 2015 recommending primary HPV testing be considered for women starting at age 25.
COMPREHENSIVE CARRIER TEST
Comprehensive Carrier Testing can inform a couple if they are at risk of having a child with certain genetic conditions. While planning a family and preparing for pregnancy, or during pregnancy, you can use the results to allow your patient to consider the most complete range of reproductive options. For many of these diseases, prevention is the only cure.
Mendelian diseases are diseases that result from a mutation at a single gene and collectively account for -20% of infant mortality and -10% of pediatric hospitalizations. Mendelian disease can manifest in a variety of ways, but many of the common disorders of interest to the obstetrician-gynecologist present in an autosomal recessive way. Hence the disease only occurs when the mutant gene is present in a homozygous state (two copies).
Preconception carrier screening has resulted in significant declines in the incidence of several severe recessive diseases such as Tay-Sachs and cystic fibrosis. Given the magnitude of carrier burden and the lower cost of testing compared to treating these conditions, carrier screening by Next Generation Sequencing may be an economical way to reduce the incidence of and ameliorate suffering associated with severe recessive childhood disorders.
WHAT IS A CARRIER?
A carrier is a person that is heterozygous for a a recessive disease gene allele but has not symptoms (or only mild symptoms) of disorder. This means he or she has inherited one normal copy of the gene and one copy that confers disease. A child of two carriers may inherit the disease if he or she gets a disease allele from each parent. The chance of two carriers having a child with disease is 25 percent.
WHO SHOULD BE TESTED?
Initially carrier testing should be done for the mother only if the mother is found to be a carrier then her partner should be tested. During pregnancy concurrent screening of the patient and her partner is suggested if there are time constraints for decisions regarding prenatal diagnostic evaluation. Testing is highly recommended if the patient: 1. Belong to an ethnic group that has high rate of carriers of certain genetic disorders. 2. Has a genetic disorder. 3. Has a child with a genetic disorder. 4. Has a family history of a genetic disorder.
WHEN SHOULD THE TEST BE PERFORMED?
Ideally carrier screening should be performed before pregnancy (preconception) to allow for a broader range of options and more time to make decisions if both partners learn they are carriers of a genetic condition they may choose to use in vitro fertilization with preimplantation genetic diagnosis (PGD) or donor egg or sperm to achieve pregnancy. They may also choose not to become pregnant or consider adoption.
Carrier screening can also be done during pregnancy at which point both partners may choose to be tested at the same time. Testing could enable perinatal diagnosis and treatment which can profoundly diminish disease severity.
WHAT CARRIER TESTS ARE AVAILABLE?
Carrier testing is available for a number of diseases including Cystic Fibrosis, Fragile X Syndrome, Sickle Cell disease, and Tay-Sachs disease. For a complete list see our Cancer & Disease page.
NON-INVASIVE PRENATAL TEST
The Non-Invasive Prenatal Test (NIPT) is a simple blood test that screens for the most common chromosomal abnormalities that can effect your baby's future health. A blood sample can be drawn in your doctor's office as early as the 10th week of pregnancy and it may help you avoid more invasive procedures such as amniocenteses or chorionic villus sampling (CVS) which are not without risks to you and your baby. The Non-Invasive Prenatal Test is available for both singleton and twin pregnancies. Test results are usually reported back to your healthcare provider in approximately 1 week.
HOW DOES THE TEST WORK?
A sample of your blood is drawn and the genetic material (DNA) from you and your baby is tested. Non-Invasive Prenatal testing uses an advanced technology to analyze millions of DNA fragments per sample and accurately count the number of chromosomes present. It then uses a special SAFeR calculation method to determine if there are too many or too few copies of these chromosomes in your baby.
WHAT KINDS OF CONDITIONS CAN THE NIPT DETECT?
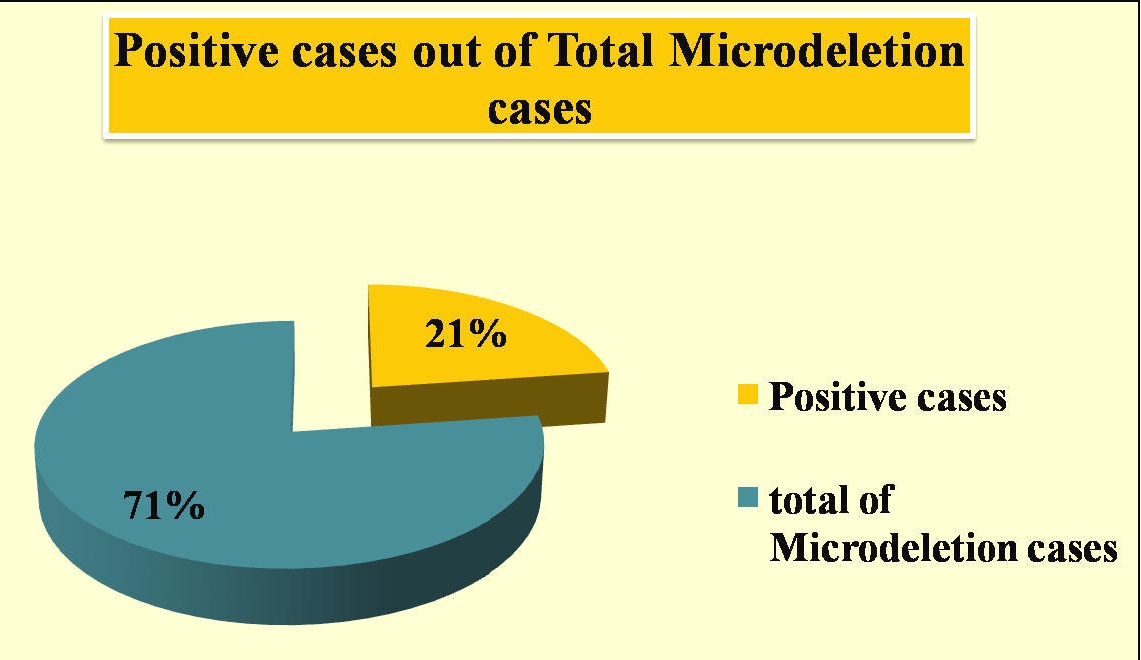
The NIPT looks for too few or too many copies of chromosomes. Chromosomes normally come in pairs. Healthy people have 23 pairs of chromosomes, the last pair of which determines sex. Men normally have an XY pair of sex chromosomes and women normally have an XX pair of sex chromosomes. Missing or extra copies of chromosomes are called "aneuploidies" and are often associated with mental or physical disabilities with different levels of severity. Basic reports contain results for chromosomes 21, 18 and 13 as well as sex chromosomes if selected. Patients also have the option to receive additional information on chromosomes 9 and 16 as well as selected microdeletions.
BENEFITS OF THE NIPT TEST
NIPT offers parents-to-be a new choice to obtain important information about the health of their developing baby. This screening test is usually offered to pregnant women identified by their doctor at risk to have a chance of fetal aneuploidy.
- Uses a simple, single blood draw from your arm - just one tube of blood is all that's needed.
- Can be drawn conveniently in your doctor's office.
- Provides reliable answers about the most common chromosomal abnormalities.
- Can test for sex chromosome conditions (for singleton pregnancies) if ordered by your healthcare provider.
- Has the lowest test failure in its class (0.1%)
Fragile X syndrome (FXS) is the most common inherited cause of intellectual disability (ID) and autism in males, and a significant cause of ID, learning challenges, and anxiety in females. The condition follows an X-linked dominant pattern of inheritance and occurs in 1/4000 males and 1/6000 females worldwide. FXS is caused by an expansion of repeating DNA segments of the base pairs CGG, called CGG repeats, in the 5' untranslated region of the FMR1 gene, located on the X chromosome. Typically, individuals have between 5-44 CGG repeats in this region. Individuals with FXS have >200 CGG repeats, which leads to absence of gene function. A molecular diagnosis of FXS can optimize medical management and treatment and provide important information for at-risk relatives.
Individuals with 55-200 repeats are FMR1 premutation carriers, with a population frequency of approximately 1/250 females and 1/1000 males. Premutation carriers do not have FXS, but are at risk for later-onset health issues including fragile X-associated tremor/ataxia (FXTAS) in a percentage of males and females, and FMR1-related primary ovarian insufficiency (POI) in some females. In addition, female premutation carriers are at risk for having a child with FXS. A molecular diagnosis of FMR1 carrier status in males or females can assist with medical management of current or future clinical symptoms as well as reproductive decision-making and family planning.
Who should get tested: Women of reproductive age who are pregnant or considering a pregnancy, and request carrier testing regardless of family history and/or Males or Females of any age with:
- unexplained intellectual disability (ID)
- autism or autism-like features
- developmental or learning problems
- cytogenetic findings consistent with FXS
- adult-onset tremor/ataxia
- female infertility associated with elevated follicle-stimulated (FSH) or primary ovarian insufficiency
- a family member with ID of unknown etiology
- a family member diagnosed with FXS
- a family member identified to be an FMR1 premutation or intermediate carrier